CASE report
By K. Brandon Strenge, MD

K. Brandon Strenge, MD
Education:
Areas of Interest:
The patient presented with right shoulder and arm radiculopathy.
He had weakness on exam in the right deltoid and biceps. The patient had no left arm symptoms at all.
The patient served in the Army and is a retired veteran.


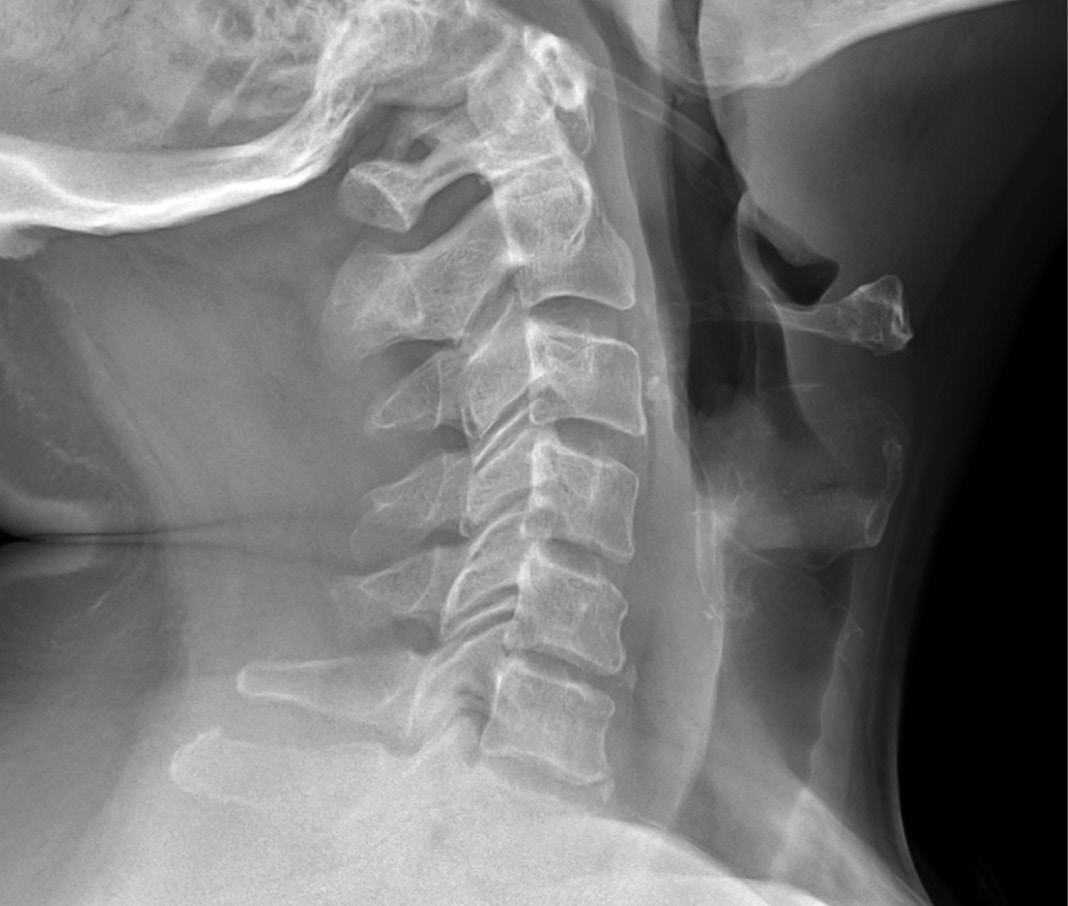
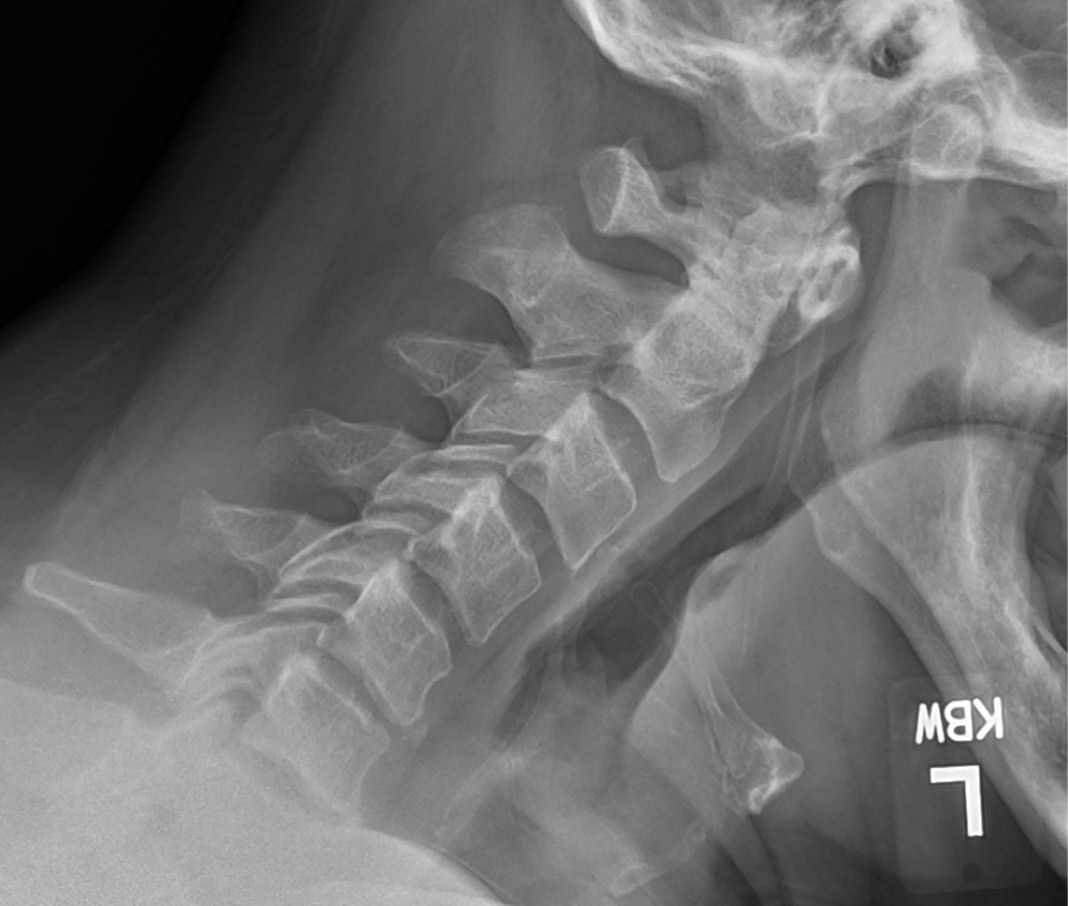
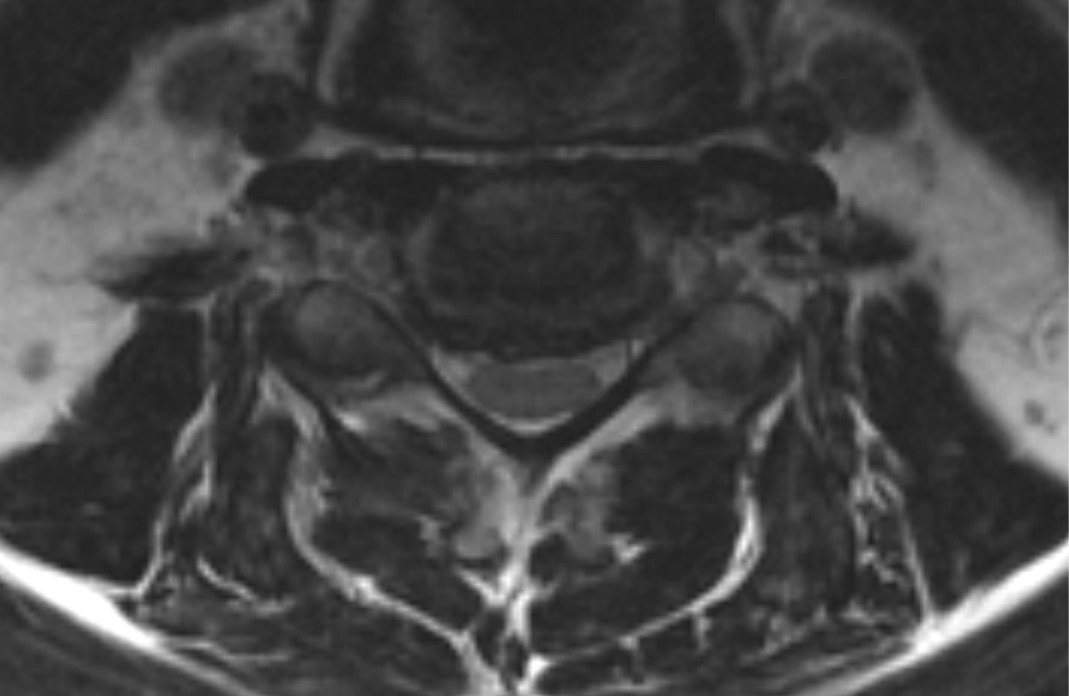
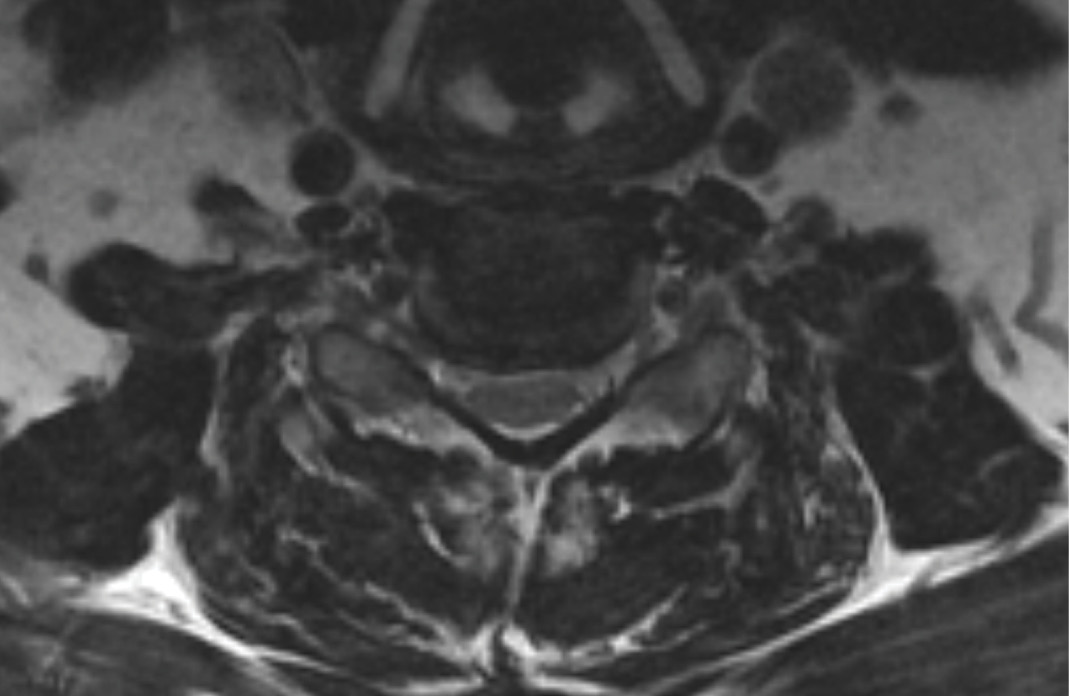
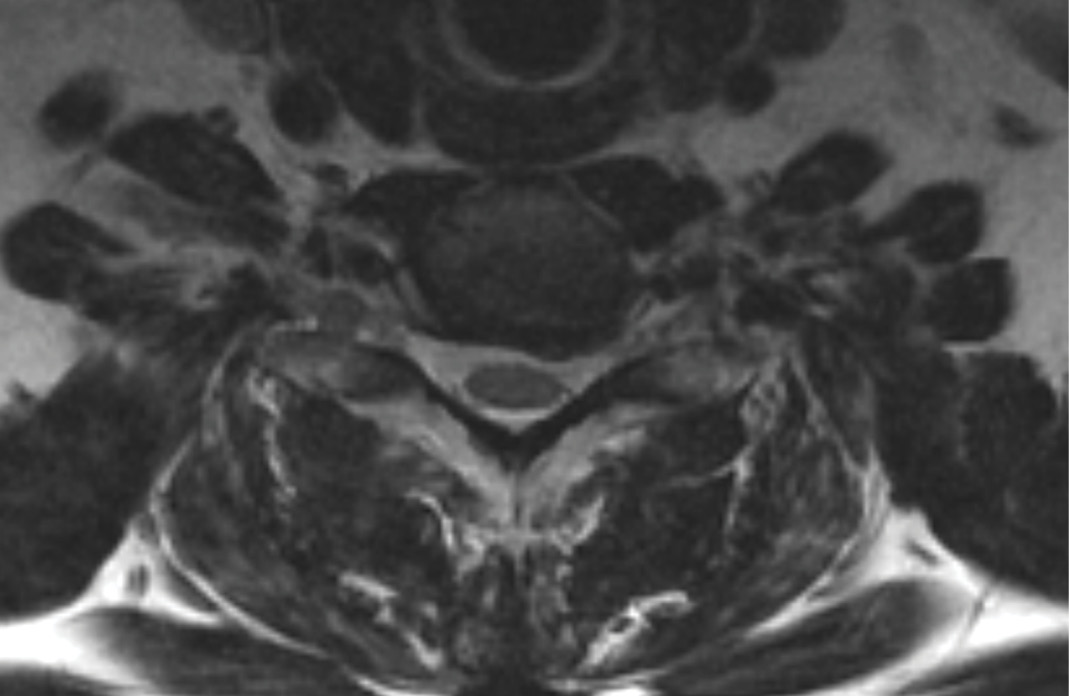
MRIs illustrated mild degenerative disc disease from C4-6 with disc herniations at both C4-5 and C5-6. The axial slice through C4-5 showed a right central disc herniation causing central and mainly right-sided foraminal stenosis. The axial slice through C5-6 showed a central disc herniation also causing central and mainly right-sided foraminal stenosis. The axial slice through C6-7 showed a left-sided disc herniation causing some left-sided foraminal stenosis, however, the patient did not demonstrate any left-sided symptoms.
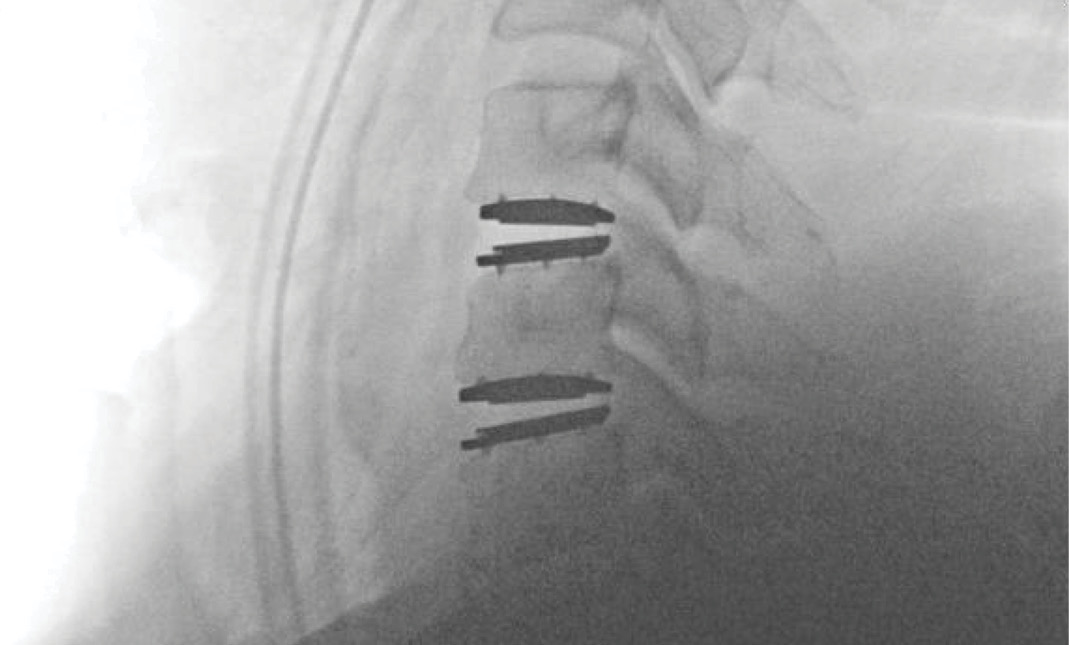
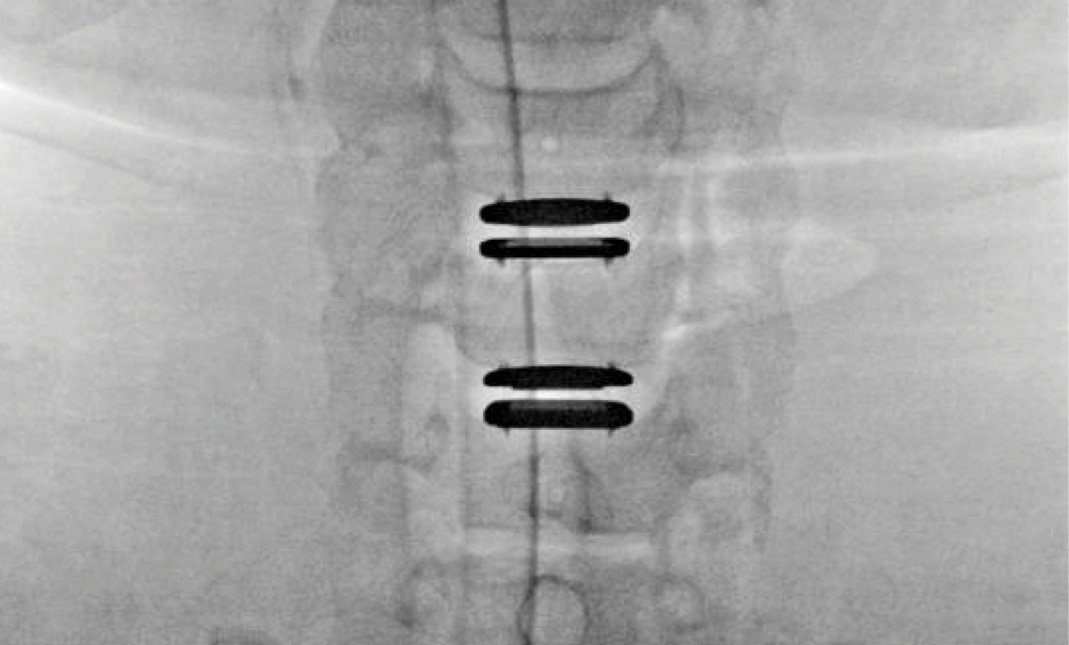
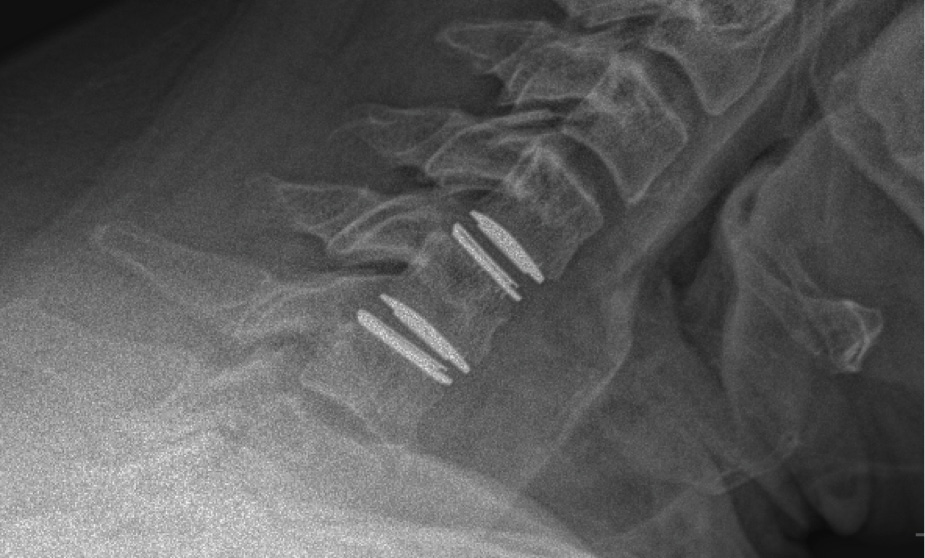
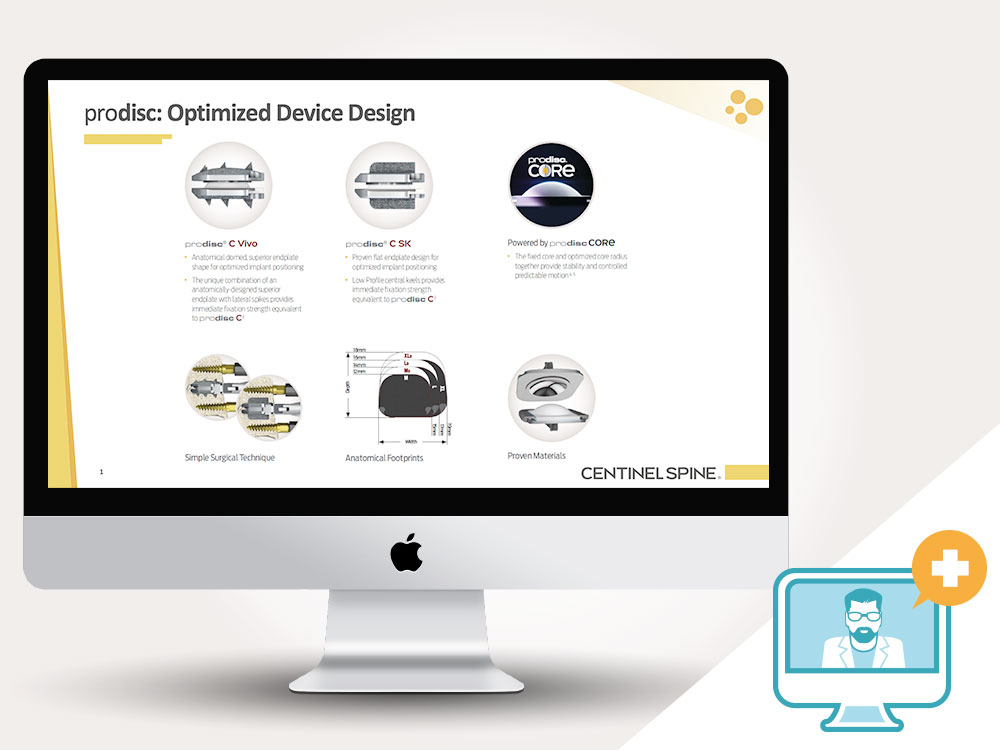
Upon examination, the patient had good motion on flexion-extension, so fusion was not considered at all. My operative plan was to use prodisc cervical devices and replace both discs at C4-5 and C5-6, giving me the flexibility to use either a domed or flat implant.
On his last office visit, 3 months post-operatively, his arm pain was gone and his strength was improving, with only slight residual weakness. He was working with physical therapy for it. All medications used pre-operatively were already discontinued at that point.


During the procedure, prodisc C Vivo fit well within the C4-5 concave endplate. I expected to use a flat endplate prodisc C SK at C5-6, however I trialed the domed prodisc C Vivo and it actually looked good, so I unexpectedly used matching implants.
It was very helpful to have the flexibility to use either a flat or a domed implant at either level. Having the different size options available to truly match patient anatomy that the Match-the-Disc™ System provides enabled me to avoid having to alter the patient’s anatomy to fit the device.
In future cases, I expect to use prodisc C Vivo to match the concavity with non-degenerated levels, and prodisc C SK for more degenerated levels, where flatter endplates may be needed. It is very useful to have a system that can adapt to the degenerated anatomy as needed.


EDUCATIONAL development
Centinel Spine offers a variety of educational programs tailored to meet the diverse training needs of physicians. Hands-on Bioskills Courses, Peer-to-Peer Webinars, and OR Surgical Observations have been designed to review patient selection, surgical technique and tips, post-operative care, and other related topics. These programs can be customized to individual physician needs, providing varied levels of support to surgeons.

About our
Hands-on Bioskills Courses
These courses provide surgeons with an educational experience focused on patient selection, surgical technique, strategies, and solutions for addressing specific spinal pathologies. The course format includes lectures, case discussions with expert faculty, and a bioskills lab.
The curriculum covers biomechanical considerations, indications and patient selection, surgical technique, tips and tricks, post-operative care, and best practices.
About our
Peer-to-Peer Webinars
Centinel Spine’s live streaming webinars provide a convenient way for physicians to learn from experts in motion preservation discussing specific treatments, techniques, and strategies for patient care.
Our interactive webinars allow participants to pose questions, receive answers, and exchange ideas in real-time with their surgeon peers from the comfort of their homes or offices.

About our
Surgical Observations
Surgical Observations are a surgical technique training and continuing education program that exposes surgeons to the technical procedures and skills required for anterior column surgery, through a combination of case discussions and viewing live surgery.
Surgeon OR Visitations are offered at Centinel Spine experienced faculty locations, where key thought leaders in spine educate with a focus on the anterior spinal column.
Watch this short primer on Centinel Spine and its unique and extraordinary place as a catalyst of change in the spine industry—with pioneering technologies and a clinical history that have led to successes ranging from PGA champions to a growing list of surgeon-patients.
Watch the Video